“I’m driving in my car and I see and smell a car burning on the side of the road. Suddenly my chest gets tight and I can hardly breathe. I smell cordite [ammunition powder]. My pulse is racing, and I start to sweat. My hands tingle. I feel the blast wave hit me.”
This is a flashback described by a soldier suffering from post-traumatic stress disorder (PTSD). His trauma came from clearing a bunker during the ground assault period of Operation Desert Storm in 1991. The sights, smells, touch, and sounds are from close-quarters killing while moving through the bunker. An inner door blew up as this soldier approached it, knocking him unconscious. In 2008, the life-threatening incident came back in full force, with the complete packet of sensory information—undiminished in intensity nearly two decades after his injuries.
PTSD is a result of an evolution-driven adaptation; human beings are hard-wired to remember life-threatening memories for our long-term survival. This is referred to as a negative bias. If a tiger came out of a cave and chased us and we survived, we would never forget that cave. It becomes a memory without a time stamp; it will remain in the present. It is a complete packet of all the sensory information associated with that incident. Elements of that sensory information packet, including the sights, sounds, and scents, can lead to a partial or complete re-experiencing of the episode. A re-experiencing—or flashback—is not a memory. It is in effect happening at that moment, with all its original intensity. Most people are quite resilient to having horrible things happen to them, but everyone has a point where they cross a threshold into PTSD. A much more potent initiator of PTSD is when a person is responsible, or feels responsible, for the traumatic incident, even in the case of justified killing in combat.
On average, at least one service member or veteran commits suicide every day as a direct result of their service. Almost certainly this is a low estimate, and this number does not begin to encompass the large number of post-deployment deaths due to PTSD-associated reckless behavior. Although most (but not all) large published studies support a strong link between PTSD and suicide, the exact number of increased suicides is subject to debate. Some studies state that veterans with a PTSD diagnosis are more than six times as likely to commit suicide as veterans without PTSD, with most studies supporting a minimum of 1.8 times as likely to commit suicide.1
The Department of Veterans Affairs released a report in September 2019 that stated there was an average of 6,000 active-duty and veteran deaths per year from suicide between 2008 and 2017.2 (That translates into 45 deaths per 100,000 veterans, versus the CDC reported figure of 13 suicides per 100,000 citizens over approximately the same period). The average number of overseas combat operations deaths per year was 378 between 2006 and 2018. There were 11 combat-related deaths in 2017.3 Even the most conservative estimates have PTSD-related suicide resulting in at least 400 additional deaths every year.
Over the past five years we have lost at least seven times as many service members to PTSD-related suicide as are lost in combat, and this number is most likely many times that.4 This is happening in the present tense. It also is happening from PTSD associated with military-on-military sexual assault and to civilians in massive numbers.
Most cases of PTSD will resolve within one year, but not all. The Department of Defense (DoD) and the Veteran’s Administration (VA) spend billions of dollars treating military members and veterans suffering from PTSD. The standard course of treatment largely has focused on psychotherapy and medication, both of which have medical evidence showing limited effectiveness.5 Fortunately, there is a new treatment method that is demonstrating a high level of effectiveness with minimal risk factors. It is called the Stellate Ganglion Block (SGB).
Stellate Ganglion Block
SGB is a safe, routine medical procedure that has been in common use since the 1940s.6 Its use in PTSD, however, is relatively new.7 Anesthesiologist Eugene Lipov and colleagues first described a successful treatment of a single case of non-combat-related PTSD with a right-sided SGB in 2008.8 Two colleagues and I were the first to use SGB to treat combat-related PTSD. Our initial results were published in 2010, followed by a case study of 166 patients in 2014.9
SGB is an injection into the front of the neck, precisely guided using ultrasound or fluoroscopy (X-ray), that targets the cervical sympathetic chain.10 This is a component of the autonomic nervous system that is a two-way information conduit between the brain and the body. SGB is referred to as a “block” because the goal of the injection is to temporarily stop the nerve condition with a dose of long-acting local anesthetic (a numbing agent like you might get before a dental filling.)
The sympathetic nervous system is responsible for your fight-or-flight response when confronted with perceived threats, such as when someone driving in front of you on a dark rainy road slams on their brakes, or when someone tries to kill you.
Chronic activation of the sympathetic (fight-or-flight) nervous system is the core pathology of PTSD and leads to a chronic stress state and anxiety. This chronic and inappropriate activation of the sympathetic nervous system is what is working against people with PTSD. However, doctors can reset this fight-or-flight response with a Stellate Ganglion Block.11
A SEAL Admits to Symptoms
“Can I ask you something, doc?”
“Shoot.” My patient was a decorated, respected Navy SEAL officer and assault team leader, and I was doing an ultrasound-guided, platelet-rich plasma injection for his chronic tennis elbow. He was a month out from leading his team on a sixth combat deployment.
“I’m having trouble remembering things, even the names of people I know well.”
“Anything else?”
“Yeah. I notice I’m drifty during important briefings, and that’s not me.”
“Kids?”
“Four kids under the age seven.”
“Do you find yourself getting mad at them, irrationally mad?”
“Yes.”
This was a patient interaction in 2012, at the time when the use of an ultrasound-guided SGB to treat the anxiety symptoms of PTSD finally started to get traction. A medical team I was part of treated nearly a third of the members of a particular SEAL Team. SGB worked well, with rapid results. Because it worked on so many special operators, we published our results in the medical literature.12 This led to other studies and papers,a featured segment on the CBS news show 60 Minutes,and in August 2019, the acceptance for publication in a major medical journal of a DoD-sponsored multicenter randomized control study that demonstrated causality between SGB and relief of PTSD symptoms.13 Back to our SEAL.
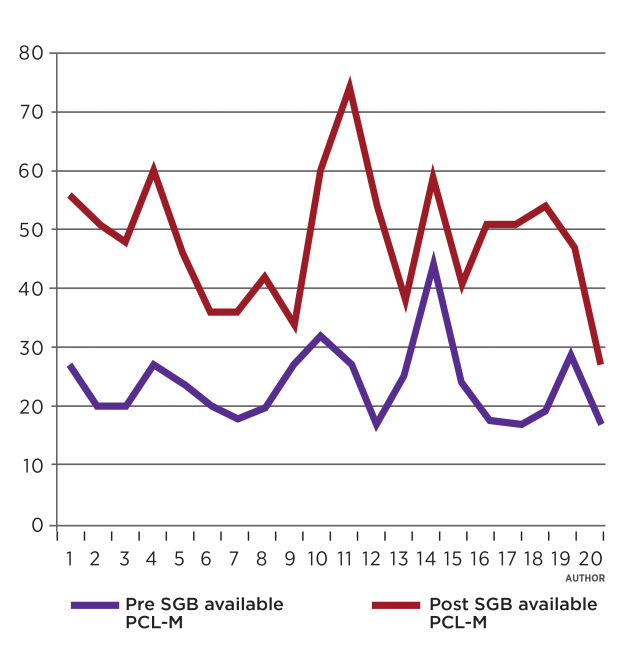
I had him fill out a PCL-M questionnaire—a standard 17-question, validated instrument to show the presence or absence of PTSD, as well as to indicate if symptoms are improving or getting worse. All SEAL operators and combat support staff at this SEAL Team filled these out upon returning from each deployment. They almost always lied on them. They said they were fine.
“This time fill it out honestly,” I said. Maybe because he knew I had been a SEAL before becoming a physician, he filled it out honestly. This time the score was clearly positive for PTSD.
“Do you want me to fix this?” I asked.
I had been using SGB sporadically to treat PTSD symptoms for three years and had published the first medical journal article on its use to treat combat-related PTSD symptoms. We did a right-side SGB on him. He had an excellent Horner’s response, which is a constellation of symptoms that gives visible proof that the sympathetic (fight-or-flight) nervous system temporarily is shut down. The next day he got in a car with his wife and four screamers and drove 800 miles for a long weekend. He was fine, he was calm, he could sleep well at night. He was himself again. When he returned to work, he gathered his assault team. He honestly addressed the issues he had been dealing with—poor memory, poor concentration, irritability and quick anger, and poor sleep.
“We are going back into combat in a month. We need each other to be at our best. If you are dealing with these symptoms, you need to get this fixed,” he told his men.
The next time I was in Virginia Beach I treated 19 SEALs in one day. Because it worked so well and quickly, every month or so I would treat another 20 SEALs, direct-support medics, and combat support staff. This all happened because of one man, Navy Captain Matt Hickey, the command surgeon for these SEALs at the time.
Matt and I had been SEALs at the same time, and we both went on to medical school. He had brought me down to his command to help treat musculoskeletal conditions, but for the next two years we mostly treated PTSD patients using SGB. Another person who was instrumental to our success was Dr. Shumi Tabassum Rahman-Rawlins, one of the command psychologists. She saw the benefits of SGB and that by working together we could help these special operators who had been asked to do so much for our country. Shumi is an exceptional clinician, and the men trusted her because of her sincere “tough-love” compassionate care.
This potent combination—a patient population who had made multiple combat deployments over a decade, a command surgeon who intensely looked out for the welfare of his people, an organic behavioral health professional who could both identify those who needed treatment and continue with follow-up care, and a physician with a technical skill that was trusted—allowed us to figure out how to help these operators who were quietly suffering with the anxiety symptoms of PTSD.
Not Just Servicemembers
It was not just the operators who suffered; their families did as well. The story was all too common; troops stretched thin resulting in multiple combat deployments with rapid turnaround between deployments and no time to truly recover. This caused their anxiety symptoms to accumulate. They largely presented as being emotionally cut off from their families and quick to anger. The immediate secondary and tertiary effects of these symptoms were often divorce and suboptimal conditions for children caught in this emotional wreckage.
Multiple medical publications estimate the PTSD prevalence for service members returning from deployments in Iraq and Afghanistan to be between 4.7 and 21.8 percent.14 These numbers are likely a significant underestimation. How did we know service members routinely lied on their postdeployment screenings? Because the numbers showed the difference.15 We compared the SEAL assault team’s PCL-M scores from their most recent postdeployment screening to their scores immediately after their assault team leader told them about his treatment with SGB. It was not a subtle difference. They went from reporting they were “fine,” with an average PCL-M score of 23.7 (which is in the normal range), to a score that clearly indicated they had significant PTSD symptoms. Their new average score was 48.25—a 100 percent increase. If these numbers even partially represent the entire group of service members who have been screened for PTSD after returning from combat, the burden of PTSD DoD-wide is an even larger issue than has been previously reported.
What was responsible for the huge shift in reporting in this group of SEALs?
It has to do with what happens to a warrior who admits having issues with PTSD after a deployment. First, there is the stigma of PTSD and asking for help. Although the military has tried to address this issue, it still exists, and it remains a barrier to treatment.16 These are proud, capable people, and asking for help does not come easily. Almost all PTSD patients feel guilty that they cannot “just get over” their symptoms. They are often highly functional in other aspects of their lives and don’t know why they cannot just “pick themselves up by their bootstraps” and move on. A vital element of treating chronic PTSD is educating patients that PTSD is a medical condition where the sympathetic nervous system has become chronically activated. Expecting them to “just get over it” is like expecting a patient to “just get over” a femur fracture or cancer.
Next, they just came back from deployment and want to get home, but if they self-identify as possibly having PTSD, they have to talk repeatedly with a behavioral health professional. Most behavioral health professionals (psychiatrists, psychologists, social workers) are perceived as being “outside the fold” and thus unable to understand what a combat veteran faced. The operators do not want to try to explain what happed in combat. The therapies can be pretty tough medicine. Many behavioral health professionals will use some variation of a treatment known as “exposure therapy,” which involves going over the trauma again and again until it loses its emotional steam. This is not just extremely unpleasant for the service member, but it restimulates the flight-or-fight reaction and has a very high dropout rate. Medal of Honor recipient Dakota Meyer, who faced direct enemy fire again and again to save his fellow Marines, stated, “Those sessions were awful to the point of being unbearable.”
Another treatment commonly offered by behavioral health professionals is psycho-active drugs such as selective serotonin reuptake inhibitors (SSRIs), which have a published response rate of 30 percent (precisely the same effect as placebo) and may have multiple adverse side effects including loss of libido.17 Is it any wonder service members returning from deployments were not seeking help?
So why did this group of SEALs suddenly answer honestly about their PTSD symptoms? Because the treatment offered, essentially a quick shot in the neck by someone they trusted, was an acceptable treatment option to them.18 It was acceptable because the effects happened immediately, because they slept better that same night, and because no one was prying into the details of what happened. SGB is not a stand-alone treatment for PTSD, but it does significantly reduce the anxiety symptoms by resetting the chronic inappropriate sympathetic nervous system tone.19 This gives the person “leg-room” to start to recover. We were often able to leverage this initial improvement to get these men to see a behavioral health professional. By reducing their chronic fight-or-flight response, we made them better able to engage with behavioral health. The combination was potent. It worked.
After we saw profound success treating SEALs, we offered this treatment to a group of Army Special Operations soldiers who had been dealing with the same long cycle of combat deployments. What we first ran into, however, was an interesting cultural difference; SEALs saw SGB worked and wanted it immediately; the Army special operators were more thoughtful in their approach to the problem. They said, “I might not be at my most optimal, but my fight-or-flight nervous system has been keeping me alive for a decade of combat. Can you guarantee this won’t hurt me somehow?” We owed them an answer.
So, we did another study and published a paper in the peer-reviewed medical literature. The study involved taking soldiers with a diagnosis of PTSD, doing a battery of eight standard neurocognitive tests on them, then, after doing an SGB, repeating the same battery of tests one hour and again one week after the block. The tests measured reaction time, memory, problem solving, and concentration. All their PTSD symptoms profoundly improved post-SGB—as we had seen in past studies. Our hypothesis was that we were not harming their neurocognitive function. The results were both surprising and extremely encouraging. Not only was there no decrease in function, we documented statistically significant improvement in the majority of neurocognitive tests, including reaction time, which was significantly improved even just one hour after the block. By extrapolating the data on published studies on the performance of law enforcement officers and athletes, we concluded SGB is the only treatment, of any kind, for any malady, that demonstrates the potential to enhance combat survivability.20
The Army soldiers were now fully on board, and rapidly saw the same benefits.21 This was because of the efforts of one of their command surgeons and my fellow researcher, Colonel Jim Lynch. Word spread, especially within the Special Operations community. To this day, SGB is widely accepted as a mainstay of treatment for PTSD symptoms in this Army Special Operations unit as well as among several other elite military organizations in DoD.
We Need to Treat More
Petty Officer John Hannon was a new SEAL in my platoon in 1990. Even in a platoon of all-stars, John was a standout. Intelligent, self-assured, witty, and hardworking, he was an exceptional SEAL. I wrote his letter of recommendation for his NROTC application. He headed off to college and came back to the SEAL community as a commissioned officer, serving with distinction and valor in multiple combat deployments. During the last few years of his life, however, he became withdrawn, even from the SEAL community, but he never sought help. He killed himself in February 2018. I wish I had known he needed help. SGB might have put him back on course.
Medal of Honor recipient Dakota Meyer has publicly acknowledged that he would not be alive today if he had not undergone an SGB for his PTSD symptoms. “If I hadn’t gotten that first SGB, I would not have been around to be a father to my daughters, I know it.” He had access to and had tried every in-patient and out-patient treatment available and had seen multiple behavioral health professionals, but nothing had helped, not even a little. Now he has had several SGBs over the past two years, and he can engage with behavioral health professionals because his sympathetic tone has been reduced. We keep in touch. He is now a successful businessman and a devoted father, and he continues to be a strong advocate for veteran care, including access to SGB.
I retired from the military after 31 years in 2018. Although I still treat many veterans, I now mostly treat civilians, including many law enforcement and emergency medical service personnel and sexual assault victims. The PTSD they have presents exactly the same as combat-related PTSD and responds to SGB just as well.
What can be done to help? SGB is available for PTSD to active-duty service members at the pain clinic at Walter Reed National Military Medical Center and at several other military treatment centers, including Womack Army Medical Center in Fort Bragg, North Carolina, and Tripler Army Medical Center on Oahu. Unfortunately, the VA treatment plan for PTSD relies heavily on pharmacologic treatment (questionable efficacy and significant adverse effects) and exposure therapy (with a published dropout rate of 50 percent). The VA published an assessment of SGB for PTSD, but despite supporting evidence, has not made SGB widely (or easily) available.22 There are currently 18 peer-reviewed papers that show SGB is safe, and all but one study showed clear efficacy. Our latest multicenter randomized controlled trial is the most powerful study to date on this topic. It took more than four years to complete, from initial funding to publication (pending). Ideally, this new evidence showing causality between SGB and relief for PTSD anxiety symptoms will prompt the VA to reassess SGB as treatment for PTSD and make it available to the VA population.
For people who cannot wait for SGB to become a widely available treatment option, it is a commonly performed medical procedure, usually done by pain medicine fellowship-trained physicians. Unfortunately, there are significant differences in how physicians perform this procedure, and this can alter how well an SGB improves PTSD symptoms. The key points are assessing the quality of the SGB to ensure the sympathetic nervous system was actually blocked and following up with patients to assess their response.23 Most insurance companies still do not consider PTSD to be an indication for an SGB, so they will not pay for it, which means out-of-pocket expenses.
Our nation has been at war constantly since 2001, and there is a cost of those wars that exceeds the scars and the limbs and lives lost. PTSD is not only a personal tragedy; it also is a massive financial burden to our country. The cost of PTSD treatment in the first year for returning Iraq and Afghanistan veterans was reported by the VA to be more than $2 billion. Health-care costs for veterans with PTSD are 3.5 times higher than costs for veterans without a PTSD diagnosis.24 Then there is the hidden burden of suboptimal lives led and lost productivity to our country from these citizens who did their duty. But this is far from a lost cause. Over the past ten years, the Stellate Ganglion Block has demonstrated the potential to significantly help large numbers of military veterans and civilians who suffer from PTSD. Now it is time to spread the word and convince the VA and other medical establishments to adopt this treatment method that is accepted by patients and actually works. As citizens, we owe it to those who suffer from PTSD to do the best we can to help them.
Extraordinary Bravery
In 2006, I was working a shift in the emergency room at the military hospital in the Green Zone in Bagdad. I was debriding the face of a military police (MP) soldier whose convoy had been hit by an IED. Fortunately, he had been wearing body armor, a helmet, and eye protection, so his face was scarred, but otherwise he was okay. As I was picking gravel out of his anesthetized face, he reached into his uniform pocket and grabbed a folded-up piece of paper—the eligibility form for a Purple Heart medal.
“Doc, can you fill this out? On the treating-physician line.”
“Wait,” I said. “You go on patrol with this form in your pocket?”
Let that sink in.
At this point the soldier’s company sergeant major arrived at his bedside.
“Sergeant Major, do all your men go on patrol with a Purple Heart form in their pocket?” I asked.
“Yes,” he stated, matter-of-factly. “It is much easier if we get the signature from the treating physician right away rather than have to track them down later.”
At the time I was the battalion surgeon for the 1st Battalion, 10th Special Forces Group (Airborne). At times I would go out with the assault teams on raids. The latent SEAL in me refused to be stuffed in the back of an up-armored HUMVEE, so I drove. We worked at night. On the way to unsuspecting targets we drove in blacked-out vehicles using night optical devices, always at the maximum speed of the slowest vehicle in the convoy, (usually over 50 mph), jinxing under every bridge and around any obstacle. Contrast this with the patrols the wounded MP had to make almost every day of his year-long deployment.
This particular MP company was responsible for route clearance. Every morning they got in their vehicles in a convoy and slowly drove the main routes around Bagdad at 15 mph, like sitting ducks, inspecting for signs of IEDs. Oftentimes the first sign was detonation. More than half the men in that company had had a vehicle blown up under them, and many of them were killed or seriously wounded. My friend, Major Al Gronewold, was an Iowa National Guardsman who had just returned from commanding a combat engineering company in Iraq on a year-long deployment. His company was also responsible for route clearance. Every man in his company had a vehicle destroyed under him, and there were many resultant cases of chronic PTSD. This was “greatest generation”-level bravery in the face of certain harm. Most Americans were unaware of the dangers facing these soldiers. At that moment, Special Forces seemed a bit less special to me compared to the gritty day-to-day bravery of the MPs.
1. J. Sareen, T. Houlahan, B. Cox, and G. J. G. Asmundson, “Anxiety Disorders Associated with Suicidal Ideation and Suicide Attempts in the National Comorbidity Survey,” Journal of Nervous and Mental Disease 193, no. 7 (July 2005): 450–54. J. L. Gradus, “PTSD and Death from Suicide,” PTSD Research Quarterly 28, no. 4 (2017).
2. “2019 National Veteran Suicide Prevention Annual Report,” Office of Mental Health and Suicide Prevention, Department of Veterans Affairs.
3. “Recent Trends in Active-Duty Military Deaths,” Congressional Research Service, 20 May 2019. Referencing DMDC Defense Casualty Analysis System report provided to CRS, 29 March 2019.
4. Gradus, “PTSD and Death from Suicide.”
5. J. Merz, G. Schwarzer, and H. Gerger, “Comparative Efficacy and Acceptability of Pharmacological, Psychotherapeutic, and Combination Treatments in Adults with Posttraumatic Stress Disorder: A Network Meta-Analysis,” JAMA Psychiatry 76, no. 6 (June 2019): 904–13.
6. H. Wulf and C. Maier, “Complications and Side Effects of Stellate Ganglion Block. Results of a Questionnaire Survey” (translated from German), Der Anaesthesist 41, no. 3 (March 1992): 146–51. D. C. Moore, Stellate Ganglion Block: Techniques, Indications, Uses (Springfield, IL: Charles C. Thomas Publisher, 1954).
7. S. W. Mulvaney, B. McLean, and J. de Leeuw, “The Use of Stellate Ganglion Block in the Treatment of Panic/Anxiety Symptoms with Combat-related Post-Traumatic Stress Disorder; Preliminary Results of Long-Term Follow-Up: A Case Series,” Pain Practice 17, no. 10 (July–August 2010): 349–65.
8. E. G. Lipov, J. R. Joshi, S. G. Lipov, S. E. Sanders, and M. K. Siroko, “Cervical Sympathetic Blockade in a Patient with Post-Traumatic Stress Disorder: A Case Report,” Annals of Clinical Psychiatry 20 (2008): 227–28.
9. Mulvaney et al., “The Use of Stellate Ganglion Block in the Treatment of Panic/Anxiety Symptoms with Combat-related Post-Traumatic Stress Disorder; Preliminary Results of Long-Term Follow-Up: A Case Series.” S. W. Mulvaney,
J. H. Lynch, M. J. Hickey et al., “Stellate Ganglion Block Used to Treat Symptoms Associated with Combat-related Posttraumatic Stress Disorder: A Case Series of 166 Patients,” Military Medicine 179, no. 10 (2014): 1133–40.
10. A. Bhatia, D. Flamer, P. W. Peng, “Evaluation of Sonoanatomy Relevant to Performing Stellate Ganglion Blocks Using Anterior and Lateral Aimulated Approaches: An Observational Study,” Canadian Journal of Anaesthesiology 59, no. 11 (November 2012): 1040–47.
11. M. R. Summers and R. L. Nevin, “Stellate Ganglion Block in the Treatment of Post-traumatic Stress Disorder: A Review of Historical and Recent Literature,” Pain Practice 17, no. 4 (April 2017).
12. Mulvaney, Lynch, Hickey et al., “Stellate Ganglion Block Used to Treat Symptoms Associated with Combat-related Posttraumatic Stress Disorder,” 1133–40.
13. S. W. Mulvaney, J. H. Lynch and R. S. Kotwal, “Clinical Guidelines for Stellate Ganglion Block to Treat Anxiety Associated with Posttraumatic Stress Disorder,” Journal of Special Operations Medicine 15, no. 2 (Summer 2015): 76–82. “SGB: A Possible Breakthrough Treatment for PTSD,” 60 Minutes, CBS, 16 June 2019. K. L. Rae-Olmsted, M. Bartoszek, and S. W. Mulvaney, “Stellate Ganglion Block for Posttraumatic Stress Disorder Symptoms: A Randomized Clinical Trial,” Accepted for publication, under embargo, in-press.
14. M. A. Gates et al., “Posttraumatic Stress Disorder in Veterans and Military Personnel: Epidemiology, Screening, and Case Recognition,” Psychological Services 9, no. 4 (November 2012): 361–82. C. W. Hoge et al., “Mental Health Problems, Use of Mental Health Services, and Attrition from Military Service after Returning from Deployment to Iraq or Afghanistan,” JAMA 295, no. 9 (March 2006): 1023–32. K. H. Seal et al., “Trends and Risk Factors for Mental Health Diagnoses among Iraq and Afghanistan Veterans Using Department of Veterans Affairs Health Care, 2002–2008,” American Journal of Public Health 99, no. 9 (September 2009): 1651–58.
15. S. W. Mulvaney, “Stellate Ganglion Block to Treat PTSD Symptoms,” Special Operations Medicine Scientific Assembly, March 2016, Charlotte, North Carolina.
16. C. W. Hoge et al., “Combat Duty in Iraq and Afghanistan, Mental Health Problems and Barriers to Care,” U.S. Army Medical Department Journal (July–September 2008): 7–17.
17. J. Difede, M. Olden, and J. Cukor, “Evidence-based Treatment of Post-Traumatic Stress Disorder,” Annual Review of Medicine 65 (2014): 319–32.
18. B. Mclean, “Safety and Patient Acceptability of Stellate Ganglion Blockade as a Treatment Adjunct for Combat-Related Post-Traumatic Stress Disorder: A Quality Assurance Initiative,” Cureus 7, no. 9 (10 September 2015): 320.
19. E. G. Lipov and K. V. Slavin, “More Evidence Supporting Unified Theory of Stellate Ganglion Block,” Medical Hypotheses 81 (2013): 146.
20. S. W. Mulvaney, J. H. Lynch, J. de Leeuw, M. Schroeder, and S. Kane, “Neurocognitive Performance Is Not Degraded After Stellate Ganglion Block Treatment for Post-Traumatic Stress Disorder: A Case Series,” Military Medicine 180 (2015): 601–4.
21. Mulvaney, Lynch, Kotwal, “Clinical Guidelines for Stellate Ganglion Block to Treat Anxiety Associated with Posttraumatic Stress Disorder.”
22. K. Peterson et al., “Evidence Brief: Effectiveness of Stellate Ganglion Block for Treatment of Post-Traumatic Stress Disorder (PTSD),” Department of Veterans Affairs, Health Services Research and Development Service (February 2017).
23. Mulvaney, Lynch, Kotwal, “Clinical Guidelines for Stellate Ganglion Block to Treat Anxiety Associated with Post-Traumatic Stress Disorder.”
24. Congressional Budget Office, “The Veterans Health Administration’s Treatment of PTSD and Traumatic Brain Injury Among Recent Combat Veterans” (February 2012).




![xpecting patients to “just get over [PTSD]” is like expecting a patient to “just get over” a femur fracture or cancer.](/sites/default/files/styles/embed_large/public/Mulvaney-PRO-11-19%20pullquote1.png?itok=OV1Q-k8E)